fasdf@sadf.tu
Food Recalls due to Listeria monocytogenes in the News Again
As we reported earlier Listeria monocytogenes was a major reason for recalls according to “summary of recall cases in Calendar Year 2016”, by the FSIS/USDA, accounting for over 80% of the pathogen recall cases. Currently, this trend is continuing, with many recalls due to L. monocytogenes. Hillcrest Dairy in Moravia NY The New York State Department of Agriculture urged consumers in Cayuga County not to consume raw milk cheeses (“Old Fashioned Raw Milk Monterey Jack,” “Horseradish Monterey Jack,” and “Chipotle Adobo Monterey Jack”) made by Ripley Dairy LLC, from Moravia, New York because they might be contaminated with Listeria. The products are packaged in a plastic shrink-wrapped and marked...
fasdf@sadf.tu
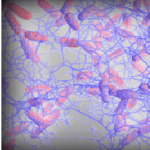
Biofilm and food safety: What is important to know?
Part 2: What are the best control strategies? Dr. Bassam A. Annous, Eastern Regional Research Center, USDA–ARS–NEA, and Dr. Ruth Eden, BioExpert. Biofilms are usually formed in a wet environment and in the presence of nutrients. Once biofilms are formed, the cleaning of the food and food contact surfaces becomes more difficult to remove the extracellular polymeric substances (EPS). Therefore, prevention of biofilm formation, using regularly scheduled cleaning and disinfecting protocols is an important first step in preventing cells from attaching and forming biofilms on surfaces. High-temperature washing can reduce the need for the physical force required to remove biofilms....
fasdf@sadf.tu
The Papaya Salmonella Outbreak Expands as Number of Victims Triples
The Recalls Since our last report on July 23, there have been several additional recalls associated with the outbreak of Salmonella in papayas. On July 26 after many people got sick, Grande Produce issued a recall for its imported papayas from the Carica de Campeche farm in Mexico. This farm seems to be the primary source of the outbreak. On August 4, a second papaya recall was issued by Agroson’s LLC, for more than 2,000 boxes of Cavi-brand Maradol Papaya imported from the same Mexican farm. A few days later, a third papaya recall was issued by Freshtex Produce. These papayas sold under the...
fasdf@sadf.tu
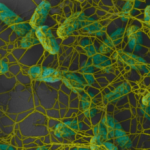
Biofilm and food safety: What is important to know?
Part 1: What are Biofilms? In nature, most bacteria do not exist as suspended (planktonic-free floating) cells. Bacteria live in a group (mass of bacterial cells) attached to each other and to surfaces, in a biofilm form. A biofilm is as a complex community of microorganisms, embedded in self-created extracellular polymeric substances (EPS). Therefore, the biofilm is a microbial population adherent to each other and to surfaces or interfaces enclosed in the matrix. In this complex biofilm network of EPS, the bacterial cells perform less as individual cells and more as a collective living system, frequently creating channels to deliver...