fasdf@sadf.tu
Another FSMA Rule Takes Effect: Foreign Supplier Verification Program (FSVP)
The FDA FSMA rule on Foreign Supplier Verification Program (FSVP) for Importers of Food for Humans and Animals is final, and the first compliance date begins on May 30, 2017. This rule imposes far reaching changes on food importers and requires review of the food safety practices of foreign suppliers and their compliance history. Foreign suppliers must be approved in advance and must have a written program before they can be a supplier in the US. The rule also requires new information to be submitted for customs entries: the FSVP importer must now be declared for each importation of FDA-regulated food (including...
fasdf@sadf.tu
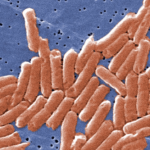
A New Method for the Detection of Salmonella in Powdered Dairy Products
The Journal of Dairy Sciences reports that a team of researchers from China (Zhao et al. J. Dairy Sci. 100:3480–3496 May 2107) developed a new method for the detection of Salmonella in infant powdered milk. The developed method is claimed to be rapid, specific, and sensitive. It is is based upon loop-mediated isothermal amplification technique combined with a lateral flow dipstick (LAMP-LFD) as the detection step. Loop-Mediated Isothermal Amplification Technique (LAMP) LAMP is a powerful new nucleic acid amplification method that detects very low levels of DNA. The method amplifies a few copies of target DNA with high specificity, efficiency and rapidity. The method uses a...
fasdf@sadf.tu
Ten Hospitalized and One Death Linked to Botulism Outbreak due to Contaminated Cheese Sauce
The Botulism Outbreak According to California state and local officials 10 people were hospitalized after they had contracted botulism from eating nacho cheese sauce served at the Valley Oak Food and fuel gas station in Walnut Grove, California. According to CNN the Sacramento County Department of Health and Human Services wrote in a statement that the cause of the illness “appears to be prepared food, particularly nacho cheese sauce” from a gas station in Walnut Grove. On May 8, health officers from the state Department of Health impounded four bags of Gehl’s cheese sauce and reopened the store to sell prepackaged food items...
fasdf@sadf.tu
Aunt Jemima Frozen Products are Recalled due to Possible Listeria Contamination
More environmental Listeria testing is being conducted due to the Food Safety Modernization Act (FSMA), resulting in more recalls due to Listeria monocytogenes found in the environment, not necessarily in the product. The FDA announced that Pinnacle Foods Inc. is voluntarily recalling a variety of flavors of Aunt Jemima Frozen Pancakes, Frozen Waffles & Frozen French Toast Slices,distributed nationally in the United States and one product distributed into Mexico. The recall is due to the potential of the products being contaminated with Listeria monocytogenes, as Listeria monocytogenes was found in the production plant environment. Two additional products (Aunt Jemima French Toast & Sausage, and Hungry Man Selects Chicken...