The FDA reported that Keeler Family Farms of Deming, NM recalled red, yellow, and white onions shipped from July 1, 2021, through August 25, 2021, imported from Chihuahua, MX, due to Salmonella. An outbreak of Salmonella in onions is being investigated. 652 total illnesses have been reported to date, including 202 hospitalizations. While investigations into various potential sources of Salmonella remain ongoing, to date, no onions marketed through Keeler Family Farms have tested positive for Salmonella. As of now, no specific source of contamination or contaminated shipment has been identified, and FDA is also investigating other potential sources of contamination and has not yet reached a conclusion. Onions were distributed to wholesalers, restaurants, and retail stores in all 50 states and the District of Columbia. The onions were distributed in 25lb/50lb mesh sacks. They contain a label marked as MVP (product of MX) but were processed at Keeler Family Farms. The last to ship was on August 25, 2021. @ https://www.fda.gov/safety/recalls-market-withdrawals-safety-alerts/keeler-family-farms-recalls-red-white-and-yellow-onions-due-possible-health-risk?utm_medium=email&utm_source=govdelivery
ruth
Keeler Family Farms of Deming, NM is voluntarily recalling red, yellow, and white onions shipped from July 1, 2021 through August 25, 2021 that were imported from Chihuahua, MX. The onions are recalled because they have the potential to be contaminated with Salmonella. Salmonella, is an organism t
The CFIA announced the recall recalling whole raw onions (red, yellow, and white) exported by Prosource Produce LLC of Hailey, Idaho, produce of the state of Chihuahua, Mexico, from the marketplace due to possible Salmonella contamination. The recall includes all batch/lots of Big Bull, Peak Fresh Produce, Sierra Madre, Markon First Crop., Markon Essentials, Rio Blue, ProSource, Rio Valley, and Sysco Imperial branded White, Yellow, and Red Whole Raw Onions from the Canadian marketplace due to suspected Salmonella. The same onions have been recalled and withdrawn from sale by the US FDA. The products have been sold in Ontario and Quebec and may have been distributed in other provinces and territories. There have been no reported illnesses in Canada associated with the consumption of these products. @ https://healthycanadians.gc.ca/recall-alert-rappel-avis/inspection/2021/76711r-eng.php
Whole raw onions (red, yellow, and white) exported by Prosource Produce LLC, produce of the state of Chihuahua, Mexico recalled due to Salmonella
ruth
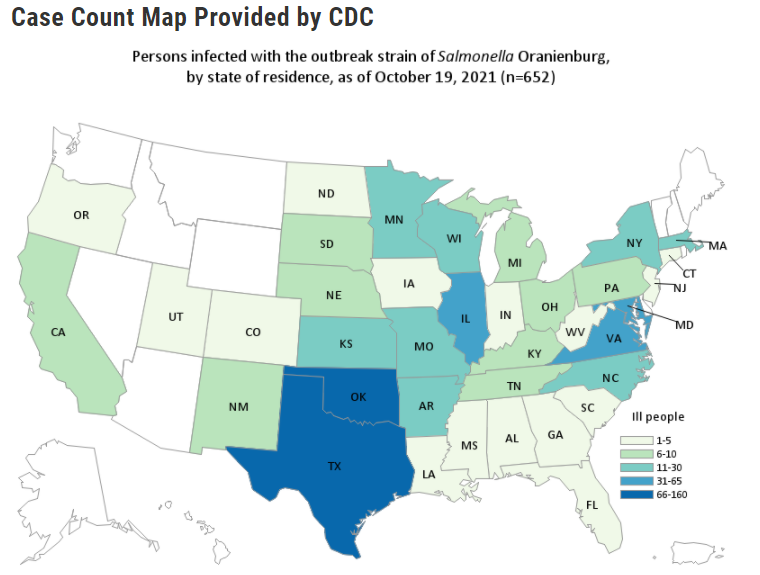
Along with CDC and state and local partners, the FDA is investigating a multistate outbreak of Salmonella Oranienburg infections linked to whole, fresh onions. The FDA’s traceback investigation has identified ProSource Inc. (also known as ProSource Produce, LLC) of Hailey, Idaho, as a source of contaminated whole, fresh onions imported from the State of Chihuahua, Mexico. ProSource Inc. has agreed to recall red, yellow, and white onions imported from the State of Chihuahua, Mexico, with import dates from July 1, 2021, through August 27, 2021. The CDC reported 652 people infected with the outbreak strain of Salmonella Oranienburg from 37 states. Ill people from the following states: Alabama 3, Arkansas 12, California 9, Colorado 1, Connecticut 4, Florida 5, Georgia 2, Illinois 37, Indiana 1, Iowa 3, Kansas 14, Kentucky 9, Louisiana 5, Maryland 48, Massachusetts 12, Michigan 9, Minnesota 23, Mississippi 2, Missouri 21, Nebraska 8, New Jersey 5, New Mexico 8, New York 12, North Carolina 14, North Dakota 4, Ohio 7, Oklahoma 98, Oregon 2, Pennsylvania 7, South Carolina 3, South Dakota 8, Tennessee 10, Texas 158, Utah 3, Virginia 59, West Virginia 1 and Wisconsin 25. There were 129 hospitalizations reported. The CDC and state and local partners identified 20 illness clusters at restaurants where onions were served. The outbreak strain of Salmonella Oranienburg was found in a sample taken from a takeout condiment cup containing cilantro and lime. The sick person reported that the condiment container also contained onions, but none were left in the cup when it was tested. Because multiple food items were present in the container and the tested sample, it is impossible to know which food item was contaminated. Descriptions of these onion types include but are not limited to jumbo, colossal, medium, and sweet onions. @ https://www.fda.gov/food/outbreaks-foodborne-illness/outbreak-investigation-salmonella-oranienburg-whole-fresh-onions-october-2021
FDA and CDC are investigating illnesses linked to whole, fresh onions. Do not eat, sell, or serve certain onions from ProSource Inc.
ruth
The FDA has issued its annual Pesticide Residue Monitoring program report FY 2019. FDA tested for 812 pesticides and industrial chemicals across 4,692 total samples, and the majority of samples had pesticide residues below the limits set by the EPA. These results are consistent with the trend of low pesticide residue violations over the past 8 years. The FDA found that 98.7% of the 1,258 domestic and 89.1% of the 3,069 imported samples complied with federal pesticide residue standards. They found no pesticide chemical residues in 42.4% of domestic and 49.4% of imported human food samples. From 365 animal food samples, the FDA found that 98.4% of the 127 domestic and 95.4% of the 238 imported samples complied. They also found no pesticide chemical residues in 40.9% of the domestic and 43.7% of the imported animal food samples. The FDA also analyzed 153 samples of domestic milk, shell eggs, honey, and game meat for pesticides. None of the samples had a pesticide residue violation except for honey, where we found 2 violative samples out of the 62 samples collected. Overall, 88.9% of the samples from this focused assignment contained no residues. @ https://www.fda.gov/food/cfsan-constituent-updates/fy-2019-pesticide-report-consistent-trends-over-past-8-years-pesticide-residue-levels-remain-low?utm_medium=email&utm_source=govdelivery
FDA has issued its annual Pesticide Residue Monitoring Program Report for FY 2019.