The EU report on antimicrobial resistance of pathogens and indicator bacteria in 2019–2020
 Introduction
Introduction
According to the WHO, antibiotic resistance is increasing to dangerous levels worldwide. Novel resistance mechanisms are emerging and spreading globally. There are numerous mechanisms reported for antibiotic resistance. In some cases, as bacteria adapt to the continuous presence of antibiotics, it becomes increasingly more resistant. Resistant bacteria are much more challenging to get rid of and control infections that they cause.
Today, the need for effective antibiotics is more critical than ever. However, few new antibiotics are in the development pipeline. Additionally, new antibiotics have shown only limited effectiveness against resistant strains. As a result, it is critical to limit antibiotic resistance so that antibiotics remain a potent treatment option against infections.
However, we see more bacteria that become “superbugs” resistant to antibiotic treatment. Since discovering penicillin in 1928, many antibiotics have been introduced. Regardless, each year more than 2.8 million antibiotic-resistant infections occur in the US.
Consequently, food pathogens should not be antibiotic-resistant. The European Center for Disease Prevention and Control (ECDC) and the European Food Safety Authority (EFSA) released a report indicating that antimicrobial resistance (AMR) in Salmonella and Campylobacter is high.
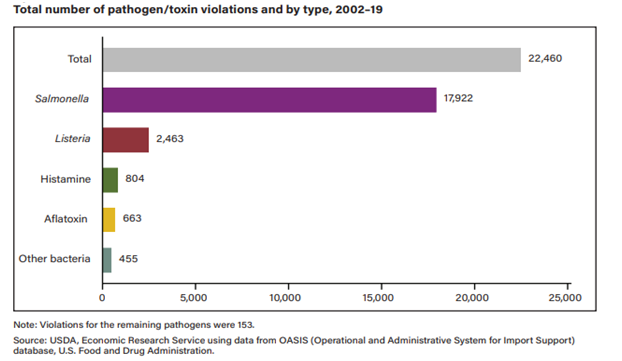
The USDA Economic Research Service published a report that indicated that in 2002–19 the products with Salmonella violations accounted for 79.8% of the rejected products, Listeria violations were 11%. Therefore it is essential to understand the antibiotic resistance (AMR) of pathogens in animals being imported into the US.
The Report content
EU report on Antimicrobial Resistance in animals, which covers 2019–2020, focuses specifically on poultry and pigs under one year old. The report of AMR in 2019–2020 included data regarding Salmonella, Campylobacter, and indicator E. coli.
27 EU Member States (MSs) submitted data on antimicrobial resistance. Resistance in Salmonella and Campylobacter from humans, animals, and food and resistance in indicator Escherichia coli and methicillin-resistant Staphylococcus aureus (MRSA) from animals and food were addressed in the report.
Antimicrobial resistance in Salmonella spp.
In 2020, salmonellosis was the second most common food-borne zoonoses in the European Union, with 54,702 confirmed human cases (a significant drop compared to 2019, most likely due to the pandemic).
For Salmonella spp. from humans in 2019–2020, resistance to ampicillin, sulfonamides, and tetracyclines was high. The resistance to third-generation cephalosporins was very low (0.8%) for cefotaxime and ceftazidime. A decline in resistance to ampicillin and tetracyclines in Salmonella isolates from humans was observed in 10 and nine countries, respectively.
In Salmonella spp. recovered from animals and food during the 2019–2020, resistance to ampicillin, tetracyclines, and sulfonamides was moderate to very high in most MSs. The resistance to third-generation cephalosporins was rarely detected.
In Salmonella spp. isolates from human cases, a moderate occurrence of resistance to ciprofloxacin was observed. Among S. Kentucky isolates exceptionally high prevalence of resistance was detected (82.0% in 2020), and in S. Enteritidis, increasing trends in resistance were observed in nine countries, both serovars predominantly being associated with poultry.
Resistance to colistin was rare among Salmonella spp. recovered from food-producing animals, although moderate resistance was observed in some Salmonella serovars.
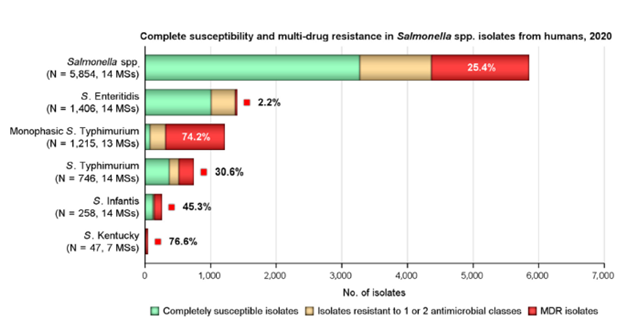
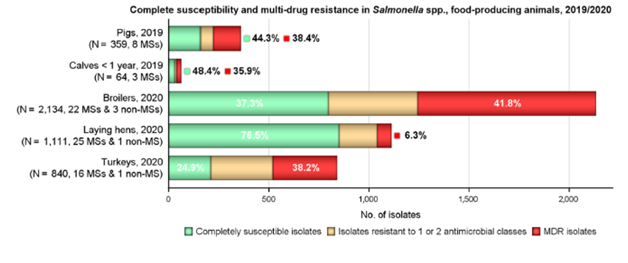
Multi Drug Resistance (MDR) was high overall (25.4%) among Salmonella spp. from human cases, most frequently observed among S. Kentucky (76.6%) and monophasic S. Typhimurium 1,4,[5],12:i:- (74.2%). Similarly, MDR was seen at very high to high levels in Salmonella spp. recovered from carcasses of broilers, pigs, and calves (53.6%, 43.3%, and 23.1%, respectively), and at a moderate level in Salmonella isolates recovered from turkey carcasses (19.1%).
Moderate to very high resistance levels to ampicillin, sulfamethoxazole, and tetracycline were reported by MSs among Salmonella isolates from all animal/carcass origins except laying hens. Overall, high levels were also observed in isolates from humans.
Among isolates from pigs, calves, broilers, turkeys, and their derived carcasses, resistance to ampicillin was generally observed at similar or slightly lower levels than those of tetracycline and sulfamethoxazole. Monophasic S. Typhimurium showed the highest resistance to these compounds across most animal/carcasses origins.
MDR varied between countries and among the animal/carcasses origins. The overall resistance levels ranged from 6.3% in laying hens to 51.2% in broiler carcasses. In Salmonella spp., the combined resistance to fluoroquinolones and cephalosporins was very low in isolates from humans and animals. Resistance was higher in some Salmonella serovars, e.g., S. Kentucky and S. Infantis.
Antimicrobial resistance in Campylobacter spp.
Resistance rates to ciprofloxacin were very high in C. jejuni and C. coli from humans and very high to extremely high in C. jejuni, and C. coli from poultry, pigs, and calves. Erythromycin resistance was either not detected or detected at very low levels in C. jejuni from humans, poultry, and calves but observed at higher levels in C. coli isolates from humans, pigs, and poultry.
From 2016 to 2020, ciprofloxacin resistance in C. jejuni from humans increased in nine countries, while erythromycin resistance decreased in five. Resistance rates differed significantly between MSs.
Rasistance rate to ciprofloxacin were very high in C. jejuni and C. coli from humans and very high to extremely high in C. jejuni, and C. coli from poultry, pigs, and calves.
C. jejuni was susceptible to ciprofloxacin, erythromycin, gentamicin, and tetracycline. Susceptibility was detected in humans (31.3%), broiler (23.0%), turkey (16.8%), and calve isolates (24.7%). For C. coli, the susceptibility percentages were 12.5%, 13.7%, 4.4%, and 21.2% for humans, broiler, turkey, and pig isolates.
Combined resistance to ciprofloxacin and erythromycin, considered critically important for treating campylobacteriosis, was generally rare in C. jejuni from humans, poultry, and calves and low to low moderate in C. coli from humans, poultry, and pigs.
The susceptibility to the four antimicrobial classes (ciprofloxacin/nalidixic acid, erythromycin, tetracycline, and gentamicin) was 20–25% for C. jejuni isolated from broilers (23.0%) and calves (24.7%) and C. coli from pigs (21.2%). The proportions were lower for C. jejuni isolated from fattening turkeys (16.8%) and C. coli isolated from broilers (13.7%). Only 4.4% of C. coli from fattening turkeys and 1.5% of C. coli from calves were susceptible to the four antimicrobial classes. Countries differed significantly in Campylobacter susceptibility. C. jejuni isolated from broilers had susceptibility to <5% in Greece, Latvia, Poland, and Portugal to>75% in Finland, Sweden, and Norway.
Antimicrobial resistance in generic E. coli
Resistance to ampicillin, sulfamethoxazole, trimethoprim, or tetracycline for generic E. coli was found in most MSs. In poultry, resistance to quinolones was ‘very high’ or ‘extremely high levels in several MSs. Significant differences in the levels of resistance were observed between countries. MDR was more common in isolates from broilers and turkeys than in those from pigs and calves.
The antimicrobials most often represented in the patterns of MDR-isolates were tetracycline, ampicillin, sulfamethoxazole and trimethoprim, and, additionally, quinolones in poultry. Combined resistance to critically important antimicrobials (cephalosporins and fluoroquinolones) was rare in E. coli in all animal categories.
Antimicrobial resistance in methicillin-resistant Staphylococcus aureus (MRSA)
A significant observation from the 2020 data was a vancomycin-resistant t isolate in meat from sheep. The isolate lacks the typical vancomycin resistance genes, and it is likely, that the increased MIC of 4 mg/L was due to multiple point mutations as described in the literature.
Key Results
In this study, Salmonella, Campylobacter, and E. coli showed low levels of combined resistance to two different antimicrobials.
Significant improvement has been made in reducing AMR in food-producing animals in several EU member states.
Resistance to carbapenem antimicrobials was rare, with less than five resistant isolates identified in the study. Resistance to carbapenem antimicrobials is of concern because they are reserved for treating severe, high-risk infections involving multidrug-resistant pathogens in humans.
