An outbreak of Salmonella Newport with decreased susceptibility to antibiotics linked to beef in the US and soft cheese in Mexico
Summary

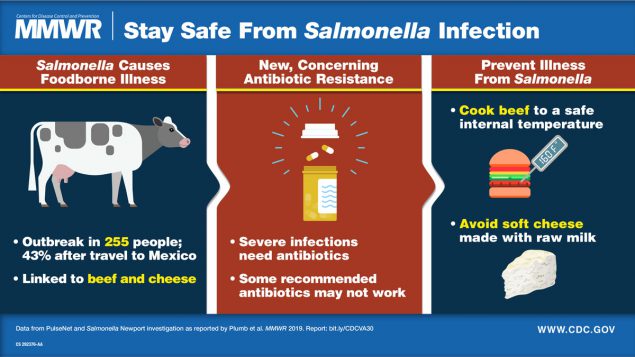
In its Morbidity and Mortality Weekly Report (MWR Weekly, August 23, 2019, 68(33);713–717) the CDC alerted the public of a dangerous strain of salmonella that has sickened 255 people and may have not responded to the antibiotics commonly prescribed to treat the foodborne infection. From June 2018 to March 2019, 255 people in 32 states were infected with the strain, with 60 being hospitalized and two dying from the bacterial infection.
The CDC claims that the antibiotic resistance of this strain of S. Newport is alarming since it covers the primary oral antibiotics used to treat Salmonellosis. The strain was resistant to ciprofloxacin and had decreased susceptibility to azithromycin. These are the two antibiotics frequently prescribed to treat Salmonella infections. Of concern is the fact that this antibiotics resistance is emerging and has not been detected before 2015.
Implications for public health
An outbreak of Salmonellosis due to multidrug-resistant Salmonella Newport, in June 2018–March 2019, resulted in 255 infections with 60 hospitalizations. The outbreak was linked to Mexican-style soft cheese obtained in Mexico and beef obtained in the United States. The CDC summarized the results in the following image:
 The CDC identified a strain of Salmonella enterica serotype Newport, in September of 2018 that was multidrug-resistant (MDR). The strain had decreased susceptibility to azithromycin, a recommended oral drug for Salmonellosis. Before 2017 less than 0.5% of Salmonella isolates had such low susceptibility to azithromycin.
The CDC identified a strain of Salmonella enterica serotype Newport, in September of 2018 that was multidrug-resistant (MDR). The strain had decreased susceptibility to azithromycin, a recommended oral drug for Salmonellosis. Before 2017 less than 0.5% of Salmonella isolates had such low susceptibility to azithromycin.
From June 2018 to March 2019, 255 cases of infection with the outbreak strain were identified in 32 states; 43% of patients reported recent travel to Mexico. In this outbreak 29% of patients for whom information was available were hospitalized, 6% were admitted to an intensive care unit, 4% had Salmonella bacteremia, and two died.
Among travelers to Mexico, the infection was connected to the consumption of soft cheese that might have been made from unpasteurized milk. Queso fresco, typically made from raw milk, was most commonly mentioned. 29% of the patients who did not travel to Mexico, reported eating Mexican-style soft cheese, and 93% reported eating beef. While the percentage who ate Mexican-style soft cheese was similar to the national average, the percentage of patients that ate beef was higher (p<0.01).
The source of the outbreak among these patients that did not travel to Mexico was identified as beef, due to the close genetic relationship between isolates from patients and beef samples. Another factor is the higher percentage of patients who ate beef, compared with the percentage of healthy persons who ate beef.
Beef might have been the source of infection among some travelers to Mexico since almost 90% of them reported eating beef, and in 2016 the outbreak strain was detected in beef imported from Mexico.
Antibiotic Resistance
From this study, 252 isolates had resistance information. 90% were resistant to trimethoprim-sulfamethoxazole, tetracycline, and chloramphenicol. 57% of the isolates were resistant to ampicillin and streptomycin and were not susceptible to ciprofloxacin (defined as the minimum inhibitory concentration of ≥0.12 μg/mL). The S. Newport strain isolated in this outbreak had decreased susceptibility to azithromycin and was not susceptible to ciprofloxacin.
Ciprofloxacin and azithromycin are the two oral drugs recommended for the treatment of Salmonella infections. The presence of the resistance genes on a plasmid is of major concern since it increases the potential for spread to other bacteria. The authors suspect that in this outbreak, 1/3 of the patients received an ineffective antibiotic.
The S. Newport strain isolated in this outbreak has emerged recently. In the NARMS surveillance report before 2016, strains with decreased susceptibility to azithromycin were not found in retail meat or animals. Two smaller multistate infections clusters of MDR S. Newport with reduced susceptibility to azithromycin were investigated among US residents; identified isolates were within 11 alleles of the current outbreak isolates during 2016–2017.
Genetic similarity was found among the isolates from beef in Mexico, and beef in the United States, suggesting that the outbreak strain is present in cattle in both countries. The report speculates that a 41% rise in macrolide use in US cattle from 2016 to 2017 (FDA report) might have caused the increase in S. Newport strain in US cattle. The authors advocate avoiding the unnecessary use of antibiotics in cattle.
